Exploiting the Ecological Arms Race
Although it might not be obvious, we are living in an ecological warzone. All around us, there is a constant battle waging between microscopic battalions which fight for survival by any means, competing over sustenance and space everywhere from the soil to our sinuses. Do not despair; the battle is (relatively) rarely targeted towards us. Most of us don’t even realise this is happening — but that doesn’t mean humanity is not involved.
The War on Bugs
Glasgow has been at the forefront of the war on microbial disease since the late 1800s. Our involvement in developing antimicrobial strategies began with Lord Joseph Lister, a professor of surgery at Glasgow Royal Infirmary, who became a pioneer of modern medicine and the ‘father of antiseptic surgery’. He studied the principles of Pasteur — the founder of modern microbiology — and applied them to surgery, becoming the first to use sterilisation techniques to lower the rate of surgical infections. In the decades following this colossal effort to eradicate microbes from the operating theatre, our focus turned to exploiting the very organisms we had first tried to eliminate. To help win the war against deadly infections we had to go behind enemy lines and make use of the natural competition between microbes. In 1928, Sir Alexander Fleming was working with a culture of bacteria which faced competition from a contaminating mould. The mould won by producing penicillin, the first isolated antimicrobial natural product. Ever since Fleming’s landmark discovery antibiotics have been our main weapon in the fight against infectious microbes. However, the ability of microbes to become resistant to current treatment strategies has driven us to seek out novel therapies, some of which exploit the interactions of our own commensal microbes.
Gut Feelings: Your Tummy Bugs and You
We share an innate relationship with the microbes which live alongside and within us. The microbiome (the collective name for the body’s home-grown friendly microbes) has been a major focus for biologists for over 20 years, and the delicate balance between man and microbe is becoming ever clearer. In understanding microbial interactions, modern medicine is taking the reins when it comes to using bacteria to combat disease, either through exploiting the natural products which microbes produce or by directly applying microbes as a therapeutic strategy1.
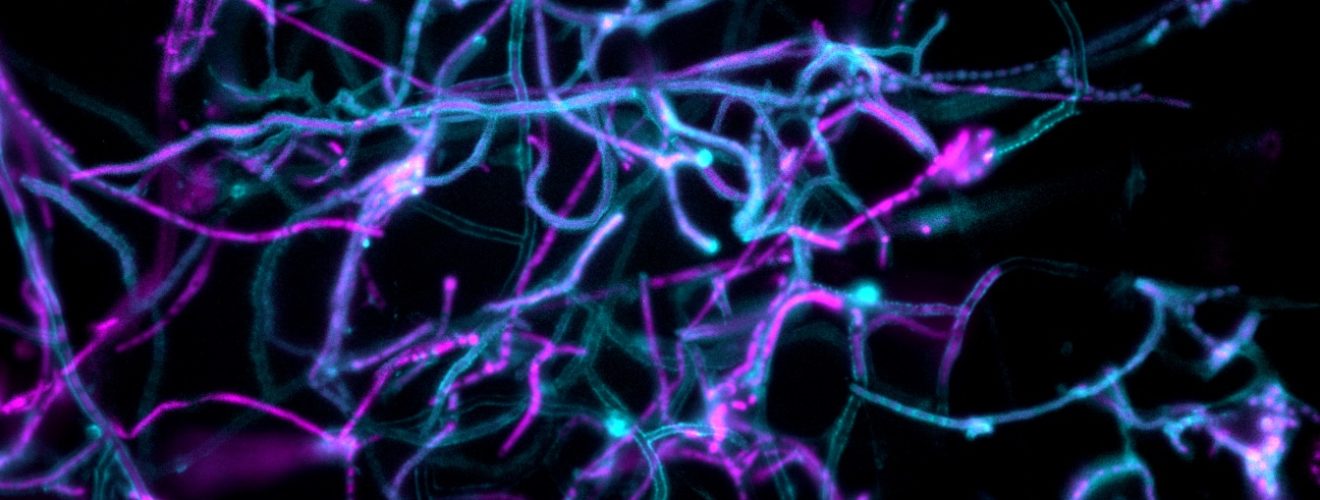
Most bacteria don’t exist as single entities. They will often either clump up into dense colonies or form thin layered sheets called biofilms, where billions of cells work together for the benefit of the community. What’s more, not only can the resident microbes carry out tasks to benefit themselves, their interactions can also be exploited by their host. An example of this is in the human gut, where the gut lining is bolstered by a layer of (mostly) friendly bacteria which help break down complex nutrients for us to absorb (of which they claim a share), while also serving to protect us from invading or opportunistic pathogens. These gut bacteria communicate with each other to share their workload, protect each other against environmental or chemical damage, and share genetic information. However, the fragile relationship between gut microbiome and host can be easily disrupted, leading to potentially severe impacts on the health of the host. Conditions such as inflammatory bowel disease, diabetes, atopic eczema and even obesity have been linked to gut dysbiosis — changes in the proportion of different microbes (dysbiosis) in the gut2. In an effort to try and restore the balance, one somewhat macabre approach has been the microbiome transplant, whereby faecal samples from healthy donors with high gut biodiversity are administered orally to sufferers of dysbiosis. Another approach relies on using bacteria-specific viruses (bacteriophage) to target specific pathogenic microbes which cause disease. The ultimate goal of both techniques is to re-establish the missing interactions between friendly microbes to restore the protective role of the gut microbiome.
The Threat of Antimicrobial Resistance
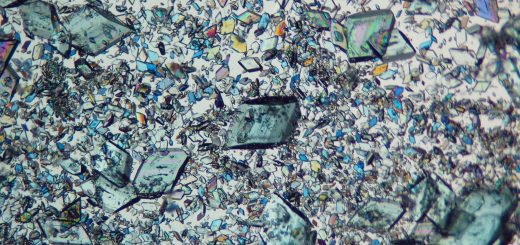
Before the discovery of penicillin, treatments for microbial infections were limited to harsh chemicals which risked deadly side effects. The introduction of penicillin and its unprecedented ability to cure infamously deadly infections revolutionised the pipeline for antimicrobial drug discovery. Research efforts turned to exploring the molecules produced by bacteria during ecological conflict, which, predictably, had the ability to inhibit the growth of competing organisms. One genus of microbes particularly talented in their ability to produce antimicrobial molecules are Streptomyces; a group of soil-dwelling bacteria. These microbes are able to produce a plethora of molecules which make up two-thirds of our clinically available antibacterial drugs, as well as some antiparasitic, antiviral and, remarkably, anti-tumour medicines. From streptomycin (the first targeted antibiotic for Tuberculosis) to neomycin in antiseptic ointment, Streptomyces have been invaluable to the medicine cabinets of the world, and their molecules have saved incalculable lives over the last seventy years.
Whilst studying bacterial interactions, we consistently bear witness to an accelerated version of the famous Red Queen theory, where organisms must constantly mutate, adapt and proliferate, not only for a reproductive advantage but merely to survive. Throughout their 450 million-year existence, Streptomyces have been trained to produce these molecules by evolution itself, whilst striving to dominate the ecological niches of soil. But equally, as the microbial underworld has evolved these warheads, their enemies have developed their own form of defence in the form of antimicrobial resistance. Antimicrobial resistance (AMR) has dominated the headlines in recent years with tales of ‘hospital superbugs’ and ‘incurable’ sexually transmitted infections. Despite only gathering public interest recently, this is, in fact, an ancient concept. For as long as there have been microbes producing chemical weapons, their targets have been evolving ways to become resistant to them. In 1945, Fleming himself warned of the dangers of AMR in his Nobel Prize speech, declaring ‘there is the danger that the ignorant man may easily under-dose himself, and by exposing his microbes to non-lethal quantities of the drug, make them resistant’.
So, the question remains: why do bacteria become resistant to antibiotics? The answer is simple — they must to survive. It is this selective pressure which provides a competitive advantage to resistant bacteria and forces the continuation of AMR genes through future generations. Therefore, without novel interventions, we are at risk of propagating the vicious circle of drug discovery followed by the emergence of resistance, as we have consistently observed over the last century. However, the ingenuity evolved by humans has left our species well-equipped to fight these battles. Innovative concepts and solutions can be found in the microbial world around us. In parts of the world, the vital bacteriophage are being deployed to fight disease, and natural microbial products are being utilised in novel ways to treat infections. Research carried out between the University of Glasgow and the University of Strathclyde have used Aurodox (a compound produced by Streptomyces goldiniensis) to prevent infections caused by deadly Escherichia coli (E. coli) O157 — the infamous ‘Burger Bug’, which is highly prevalent in Scotland. In one recent case, 22 audience members of the ‘Top Gear Live’ show at the SSE Hydro became severely ill after eating contaminated burgers. A novel ‘anti-virulence’ strategy was undertaken, wherein Aurodox was not used to kill or inhibit the growth of the infecting organism, but simply to prevent it from harming the host while in the body. Without the threat of death, the selective pressure on the bacteria for resistance is reduced and can perhaps enhance the longevity of this new treatment3.
War — What is it Good for!? (Huh!)
In fact, bacterial warfare appears to be vital to the survival of the human species. From the protection conferred from the host’s gut microbiome to the natural products produced by soil-dwelling Streptomyces, there is no doubt that our ability to exploit these microbial interactions has increased life expectancy and made our world a safer place. No longer should we have to worry about a life-threatening infection from a seemingly innocent paper cut. However, the ability of microorganisms to defend themselves against the latest ecological weapons should not be overlooked. The next few years are vital if humanity is to win not only the battle but also the war.
This article was specialist edited by Kirstin Leslie and copy-edited by Annie Hackland.
References
- This concept isn’t particularly new, and for a full overview check out the principles of Hamiltonian medicine (https://doi.org/10.1098/rstb.2013.0366), where microbial co-operation and competition are manipulated for the benefit of health.
- For more information on this check out “Missing Microbes” by Martin J. Blaser
- For more information see https://doi.org/10.1128/IAI.00595-18