Night Owl? Blame thy Genes!
It’s 7:20 A.M. The alarm clock has been blaring for the past 20 minutes. After snoozing it an innumerable amount of times, you finally manage to get out of the bed, with a nagging feeling that your sleep wasn’t complete enough. Your family blame it on your late-night gaming or reading habits, but even when you try sleeping early, you just can’t. You constantly feel that you are in the wrong time zone. Well, if you experience this, then you belong to the 10% of the world population who suffer from ‘Delayed Sleep Phase Syndrome’ (DSPS).
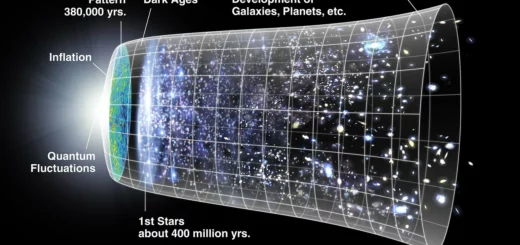
The circadian clock controls our daily bodily routine. It’s the body’s internal clock operating in every cell and tissue to align the daily changes in our biochemical, behavioural, and physiological activities with the 24-hour environment cycle. In people with DSPS, this clock runs two or more hours slower than the ordinary time, and this alters their sleep-wake cycle. They would fall asleep at 1 A.M. instead of 11 P.M. even if they are devoid of any external disturbances like artificial light or smartphones/late-night entertainment. The youth often label themselves as ‘night owls’, and this is usually a result of their incessant after-dark internet trawling. Although, the environment isn’t the only factor influencing your circadian rhythm: your genes also play a part. Variations in the genes related to your circadian rhythm can result in DSPS. A recent study published in the journal Cell describes two variations in the CRY1 gene associated with DSPS1.
Our body clock functions in a natural gene-led feedback loop. The BMAL1, CRY1, CRY2, PER1, PER2, and CLOCK genes control our circadian clock2. Proteins are created by their respective genes through transcription and translation, or gene expression. CLOCK and BMAL1 are activators – which are proteins that increase gene expression. As our body clock starts, CLOCK-BMAL1 form a complex, which drives the expression of the genes CRY and PER. In turn, the proteins CRY and PER accumulate, these proteins are inhibitors, which after a time-lag, stops the activity of the CLOCK-BMAL1 complex. These inhibitors are slowly degraded by our cells, which allows the levels of the activators to rise again, thus resetting our body clock. In people with the identified variation in the CRY1 gene, an over-active protein is produced which binds to the activators for a longer time, thereby delaying the start of your body clock. The delay in the circadian rhythm of the afflicted individuals is roughly 30 minutes – thus, their cells have a 24.5-hour daily cycle instead of 24 hours. Resulting in a 2 to 2.5-hour delay in the sleep timing of the individuals.
However, not all DPSD cases are attributable to these genetic variations. Understanding the complexity of the human genome is a key to gain insight on why even the same mutation in different people can lead to a variable manifestation of the same disorder. The environment also plays a key role in the manifestation of DPSD as it shapes our epigenome – which controls how our genes are expressed. Diseases associated with this condition include depression, anxiety, and diabetes (apart from the constant lethargy). It is important to understand the causes and thereby develop a potential treatment for DPSD as this condition leads to many long-term adverse health effects.
Edited by Richard Murchie
References
- Patke, Alina, et al. “Mutation of the Human Circadian Clock Gene CRY1 in Familial Delayed Sleep Phase Disorder.” Cell 169.2 (2017): 203-215.
- Ye, Rui et al. “Dual Modes of CLOCK:BMAL1 Inhibition Mediated by Cryptochrome and Period Proteins in the Mammalian Circadian Clock.” Genes & Development 28.18 (2014): 1989–1998. PMC. Web. 21 Apr. 2017.