The Fast Way to Cure Diabetes
Diabetes is a severe metabolic disease characterised by the failure of our body to maintain normal glucose levels in the blood. If untreated, high blood glucose can lead to several long-term complications like heart disease, kidney failure, damage to the eyes and foot ulcers. Nowadays, patients can administer insulin injections or other medications, such as insulin secretagogues or alpha-glucosidase inhibitors, to help them manage blood glucose levels. However, these treatments can cause blood glucose to drop too low, resulting in coma or even death. Diabetes is a global problem, with 422 million people diagnosed with diabetes in 2016 according to the World Health Organisation. This is predicted to double by 20301.
Diabetes can be divided into two subtypes: type 1 (T1D) and type 2 diabetes (T2D). T1D has both genetic and environmental causes, is more common in young people, and is often called ‘juvenile diabetes’. T1D occurs when our immune system cells destroy the beta cells that are present in the pancreas by mistake. These cells are responsible for producing insulin following a meal. This triggers glucose absorption in peripheral tissues, like muscle and the liver, to reduce our blood glucose levels. In contrast, T2D constitutes 90% of diabetes cases and is primarily caused by a combination of obesity, a lack of physical exercise, and contributing genetic factors. Unlike T1D, the pancreas of patients affected by T2D still produces insulin during the early stages of the disease. However, cells become ‘insulin-resistant’. This is when cells normally sensitive to insulin fail to respond to increased blood insulin levels and fail to take up glucose from the blood.
Treating diabetes globally is expensive, with $612 billion (US) spent on the disease in 2014. In the UK, approximately 3.8 million people are diabetic and the NHS is predicted to spend £16.9 billion on diabetes by 2035, that’s 17% of the total budget2. Clearly, we need to change our lifestyles, but researchers also need to improve quality of care and life for diabetic patients, whilst reducing healthcare expenditure.
Recently, the scientific community has started to realise the benefits of controlled food deprivation. During food deprivation, our body saves energy by breaking down specific tissues; reducing total energy consumption. Interestingly, once we return to a normal diet, the tissues of several systems regenerate via activation of stem cells. Researchers found that two or three days of controlled fasting can help cancer patients to overcome some side effects of chemotherapy through stem cell regeneration, producing new blood and immune cells.
Based on these results, and considering the loss of insulin-producing beta cells is a feature of diabetes, Prof. Valter Longo investigated if food deprivation can help regenerate these faulty beta cells. To avoid the side effects of prolonged fasting, the researchers developed a so-called ‘fasting mimicking diet’ (FMD). This diet is low in calories, protein and carbohydrate, but high in fat; the effects of which are comparable to a water-only diet. Prof. Longo and colleagues used a mouse model that mimics T2D, which is insulin-resistant in the early stage and shows beta cell dysfunction in the late stage of the disease. Putting the mice on FMD for four days a week lead to the restoration of beta cell function and reduced blood glucose levels. The mice were able to produce insulin again, and their insulin resistance was reduced. The researchers suggest that the FMD’s ability to promote beta cell regeneration in the pancreas whilst improving insulin sensitivity could be a therapeutic strategy to mitigate the late symptoms of T2D, reducing patient mortality rates.
In addition, the FMD was tested in a T1D mouse model, where the concentration of glucose in the blood returned to almost normal levels after two months of receiving FMD cycles. Similar to the results obtained with the T2D model, the beneficial effects of FMD in the T1D model were due to the activation of beta cell regeneration.
During FMD cycles, the number of pancreatic beta cells begin to decrease, but once the FMD is stopped and mice return to a normal diet, a series of genes involved in cell differentiation and replication are activated. One of these genes is Neurogenin 3 (Ngn3), which activates beta cell proliferation in the mouse model, leading to an increase in insulin-producing cells. Since Ngn3 is also involved in beta cell development in humans, the researchers wondered whether the FMD could have the same beneficial effects in diabetic patients.
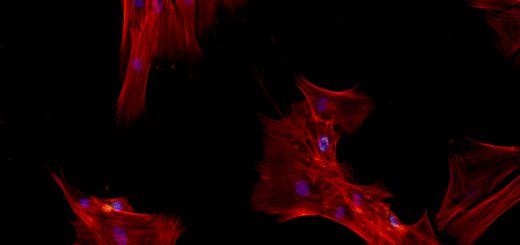
To test this hypothesis, fasting experiments were performed on pancreatic cells from healthy donors and those with T1D. Cells are cultured in nutrient rich solutions, and removing specific nutrients can mimic starvation or fasting. This induced fasting stimulated insulin production in cells from both healthy and T1D donors, which was driven by the activation of the Ngn3 gene3.
Despite the study’s promising outlook on diabetic treatment, we cannot be certain that diabetic patients would respond identically to the mouse model. A fasting mimicking diet potentially represents a valid alternative to beta cell transplantation and cell-based therapy for the treatment of both types of diabetes. Like all medical breakthroughs, we need to wait for further clinical trials to be sure that fasting is a realistic treatment for diabetic patients before we shout ‘Eureka!’.
This article was specialist edited by Jiska van der Reest and copy edited by Emily May Armstrong.
References
- http://www.who.int/diabetes/global-report/en/
- https://www.diabetes.org.uk/About_us/News_Landing_Page/NHS-spending-on-diabetes-to-reach-169-billion-by-2035/
- https://www.cell.com/cell/fulltext/S0092-8674(17)30130-7