Conquering K2: The Challenges of Synthetic Cannabinoids

With increasing frequency, the media are highlighting the concerns of various divisions of society over so-called “legal highs”, “K2”, “Spice” and “Novel Psychoactive Substances (NPS)”. With varying levels of accuracy, these terms often refer to synthetic cannabinoids. Spokespeople for agencies such as Her Majesty’s Inspectorate of Prisons, the NHS, police forces and parents of users have expressed frustration and disdain at the widespread presence and accessibility of such substances. So why, it is repeatedly asked, are they not removed from society? The answer to such a question is multifaceted.
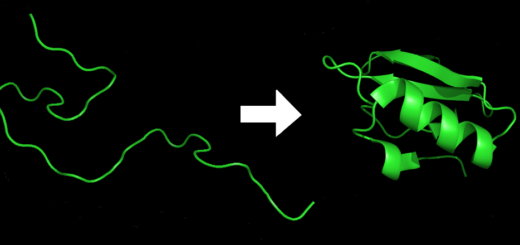
Synthetic Cannabinoids are more accurately referred to as Synthetic Cannabinoid Receptor Agonists (SCRAs). They were originally developed in the 1960s with the intention of elucidating immune responses, as some endogenous cannabinoids are known to play a role in modulating these 1. This activity takes place at Cannabinoid Receptor 2 (CB2) receptors in the immune and peripheral nervous systems. Due to structural similarities, SCRAs also bind to Cannabinoid Receptor 1 (CB1) receptors in the central nervous system, causing the psychotropic effects more commonly associated with cannabis use. These substances have been structurally adapted by drug chemists to be more potent at the CB1 receptor than natural cannabis, and this causes physiological issues.
The most psychologically active compound within cannabis is Δ9-tetrahydrocannabinol (THC), which has higher efficacy at the CB1 receptors than CB2. On its own, the effects of THC can include hallucinations, psychological distress and seizures. Within the cannabis plant, other natural cannabinoids such as cannabidiol actually have an antagonistic impact to THC, and can inhibit psychosis and seizures. This means that if an SCRA exhibits high potency at the CB1 receptor, it is not necessarily also going to bind at the CB2 receptor, resulting in no reduction of the dangerous effects of CB1 binding.
The number of SCRAs has been reported to be over 400, classed within several structural groups 2. Pharmacological assessments and toxicity testing has presented an enormous challenge given the high number of compounds, a lack of available reference standards, and ethical problems associated with administration studies. It is therefore incredibly difficult to assess the potential danger associated with their use or the significance of their detection in a clinical or forensic toxicological setting.
Scientifically proving the danger to health of each compound, in order to prohibit them, is almost impossible. While internationally published literature is now providing blood and urine concentrations for individual drugs found in cases of drug-impaired driving, hospital admissions and post-mortem investigations, the sheer variety of compounds can make this information of limited relevance. In addition to this, the trends of different SCRAs used between regions and countries can mean that what is frequently found in the UK, for example, may not be seen in the USA or Germany. Moreover, the nomenclature of the drugs doesn’t follow a universal system, so the same drug can be known by a different name elsewhere, unless there is reference to the lengthy systematic name set by the International Union of Pure and Applied Chemistry (IUPAC).
The complicated nature of the names (and they are often downright unpronounceable: MDMB-CHMCZCA, for example) is presumably why the media make reference to SCRAs as “legal highs”, “NPS”, “Spice” and “K2”, the latter two being brand names of some of the original products. This can lead to misunderstanding and a lack of distinction between other types of NPS, such as the stimulant synthetic cathinone mephedrone. Whilst entirely understandable, this does not promote communication between the general public and researchers in the field.
However, what appears to be clear is that SCRAs, in general, are contributing towards harm both from a physiological and societal point of view. There is no shortage of reports of adverse physiological reactions to these drugs in scientific and official literature, and the inclusion of the presence of an SCRA in causes of death is increasing 3, 4, 5, 6, 7. Various groups associated with custodial institutions have expressed deep concern over the prevalence of SCRAs within the prison system, with one inmate estimating that 90% of the population of one prison were abusing the drugs 8, 9, 10, 11. Reports state that abuse is leading to hysterical outbursts from prisoners who have ended up harming themselves and others. The smoking of SCRAs in prison has also been linked with illness amongst staff working with the users 12. It should be noted that the ability of equipment used currently in prison drugs screens to detect SCRAs is unknown, and no reports of the real prevalence of these drugs in custodial institutions is available.
Until this point, the legal management of SCRAs has been through the use of Temporary Drug Class Orders, which banned named compounds as and when their potential harm became apparent. This has arguably resulted in proliferation in the number and diversity of the compounds available through the synthesis of legal alternatives to banned substances. However, the implementation of the Novel Psychoactive Substances Act on the 26th May 2016 made the production and distribution of SCRAs a criminal offence. Possession of SCRAs whilst within a custodial institution will also be illegal, although possession for the rest of society will not be prohibited.
Although the complications concerning the understanding and management of SCRAs are varied, the approach taken to clarify and overcome them by the scientific community is forthcoming and robust. Researchers are gathering intelligence from non-targeted analysis of seized drugs and conducting receptor binding studies and metabolic profiling on the most frequently encountered compounds. The prevalence and effects of use within different cohorts is being documented. Regarding the potential for harm, reports of adverse effects, clinical and post-mortem drug concentrations are adding to the bank of data. As a result, the increasing understanding of the danger SCRAs pose to society can allow scientists to liaise with legislators to develop sensible policies, and medical facilities to provide optimum care for those negatively affected by SCRAs.
This article was specialist edited by Miruna Costreie and copy edited by Kim Wood
References
- Mills B, Yepes A, Nugent K. Synthetic Cannabinoids. Am J Med Sci. 2015;350(1):59-62.
- Winstock AR, Barratt MJ. The 12-month prevalence and nature of adverse experiences resulting in emergency medical presentations associated with the use of synthetic cannabinoid products. Human Psychopharmacology: Clinical and Experimental. 2013;28(4):390-3.
- Behonick G, Shanks KG, Firchau DJ, Mathur G, Lynch CF, Nashelsky M, et al. Four Postmortem Case Reports with Quantitative Detection of the Synthetic Cannabinoid, 5F-PB-22. J Anal Toxicol. 2014;38(8):559-62
- Westin AA, Frost J, Brede WR, Gundersen POM, Einvik S, Aarset H, et al. Sudden Cardiac Death Following Use of the Synthetic Cannabinoid MDMB-CHMICA. J Anal Toxicol. 2015.
- Shanks KG, Clark W, Behonick G. Death Associated With the Use of the Synthetic Cannabinoid ADB-FUBINACA. J Anal Toxicol. 2016:bkv142.
- Tait RJ, Caldicott D, Mountain D, Hill SL, Lenton S. A systematic review of adverse events arising from the use of synthetic cannabinoids and their associated treatment. Clin Toxicol. 2015:1-13.
- Christie R. EU Early Warning System Alert: Subject: 2 deaths and 3 non-fatal intoxications in Germany associated with MDMB-CHMICA (methyl-2-(1-(cyclohexylmethyl)-1 H-indol-3-ylcarbonylamino)-3,3-dimethylbutanoate). EMCDDA; 2015.
- The Centre for Social Justice. Drugs in Prison. London; 2015.
- Her Majesty’s Inspectorate of Prisons. Changing Patterns of Substance Misuse in Adult Prisons and Service Responses. London; 2015.
- The Rehabilitation for Addicted Prisoners Trust. Tackling the Issue of New Psychoactive Substances in Prisons. London; 2015.
- Prisons and Probation Ombudsman. Learning Lessons Bulletin Fatal Incident Investigations Number 9. 2015.
- Prison officers ‘falling ill after inhaling legal highs used by inmates’. The Telegraph. 2016 2016-01-18. Accessed 8th May 2016. Available from: http://www.telegraph.co.uk/news/uknews/12106476/Prison-officers-falling-ill-after-inhaling-legal-highs-used-by-inmates.html