Bacteria and the brain: A new insight into mental health
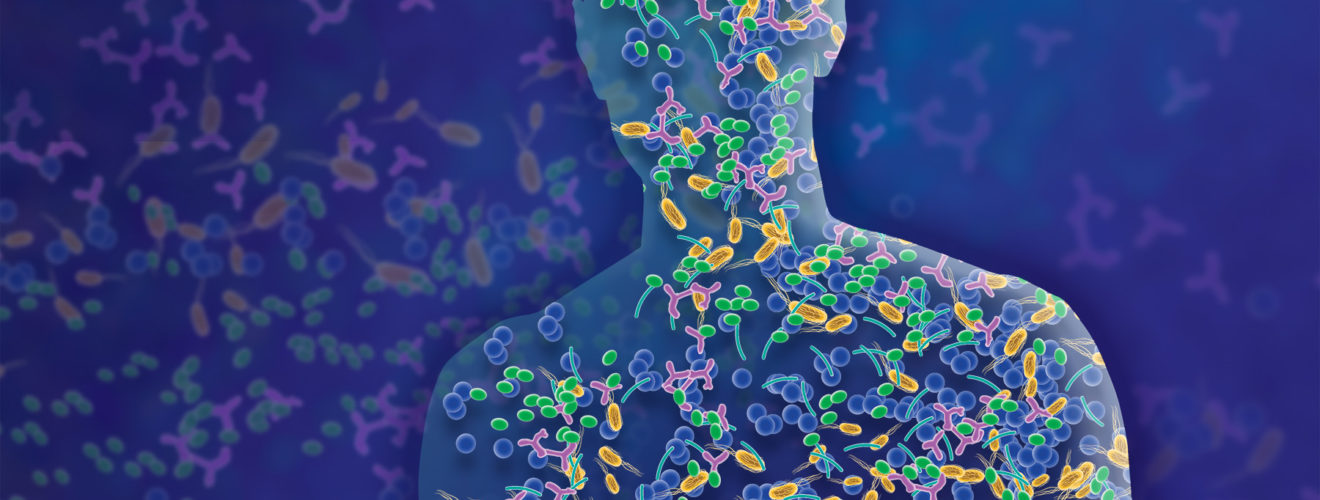
For some time now, there has been an understanding that the bacteria in your gut (termed your gut microbiota) are involved in many biological functions; from helping with digestion, to regulating your immune system, to affecting signalling in your brain. By extension, certain gut bacterial species have been linked to increasing your risk of developing various medical disorders. This has led to a huge rush in research to uncover differences in the gut microbiota of healthy and unhealthy people, and whether we can alter this to develop new treatments.
In 2004, Japanese biologist Dr. Sudo first proposed a close connection between the gut microbiota and our most complex and elusive organ – the brain. Later, this was coined the gut-brain axis. Sudo found that mice without any gut bacteria had an exaggerated stress response, suggesting a link between the bacteria and how the brain processes stressful stimuli. This ground-breaking discovery led to many other studies drawing a link between the gut microbiota and brain development, ageing, mood disorders, learning difficulties, and even Alzheimer’s Disease.
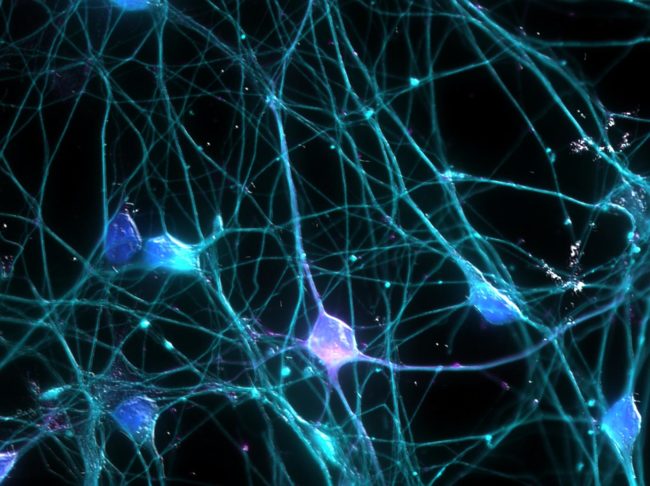
So, how are the brain and the gut linked? The answer – lots of ways. Currently, it is thought that the dominant connection is via proteins produced by bacteria. For example, some bacteria produce a molecule called brain neurotrophic factor that affects neuronal growth. Other bacterial proteins can modulate connectivity between different brain regions (affecting learning and memory), dampen or worsen inflammation, and aid in production of important brain proteins. For example, certain bacteria can metabolise precursors for serotonin, a protein implicated in both happiness and depression. The gut is also directly connected to the brain via bundles of neurons which allow direct communication between them. Some researchers even propose that the body’s immune system recognises certain species of bacteria in the gut, and sends its own signals to the brain. The complexity of the connection between the gut and the brain makes it both a fascinating and challenging field to study. To find out more on the gut-brain axis, check out this Ted Talk[1].
So how do we link brain functioning to bacterial species? Well, there are several methods. The method used by Sudo and his colleagues involved germ-free mice. Behaviour and cognitive ability differences were tested in mice without gut bacteria, and mice with normal compositions. Antibiotics can also eliminate certain bacteria to identify specific roles for different species of bacteria. Finally, in humans, scientists often look at stool samples. When you go to the toilet, DNA or RNA from the gut bacteria is shed with your faeces. This DNA or RNA can then be analysed to identify the bacterial species which it came from, and therefore which bacteria are present in your gut. These techniques have allowed us to understand the relationship between the gut microbiota and brain activity.
We’ve established that the gut microbiota affects the brain, but how does it increase your risk of different disorders, and how can we use this in treatments? Key clues for this come from the role of gut bacteria in your early years. Your gut microbiota begins to develop from birth and is mostly settled in composition by the time you hit your third birthday. This also happens to be a hugely important phase of your life for brain development and other crucial milestones such as learning to walk and talk. This correlation led to the idea that your gut bacteria may affect how well you develop, and therefore may also play a role in conditions where development is disrupted, such as autism. Indeed, in 2019, Caltech researcher Sharon G. and colleagues found that transferring the bacteria typically seen in the guts of autistic people to a ‘neurotypical’ mouse caused that mouse to exhibit autism-like symptoms. Even more intriguing was their discovery that the neurodivergent behaviours of austistic mice models could be altered by changing the gut microbiota, pointing to potential treatments for learning difficulties in general. Although these findings suggest a link between the gut microbiota and brain development and/or autism, it’s still a highly active field of research. Like to know more? Check out this video from the Diagnostic Solutions Laboratory on the importance of gut bacteria in autism[2].

Later, in adulthood, the gut microbiota may also play a role in your risk of developing mood disorders such as anxiety and depression. For example, one study showed that mice who were given the bacteria of a human patient with major depressive disorder appeared to develop behaviour associated with depression. However, mice with reduced gut bacteria diversity were also found to be more likely to develop anxiety and depression. These findings could suggest that both a lack and an excess of certain bacteria may predispose individuals to poor mental health, at least in rodents. Recently, a study identified the ‘depressive profile’ which suggested 47 different species of gut bacteria proposed to be in excess in patients with depression, compared to a healthy control. These findings are still speculative, and largely suggest correlation, not causation, but could provide new insight into these highly debilitating disorders.
Finally, at the other end of life, gut bacteria have also been proposed as a contributor to ageing, and to the development of neurodegenerative diseases. One potential role of gut bacteria is their activation of specialised immune cells in the brain, called microglia. These immune cells are known to divide excessively in old age and erroneously attack the brain itself, rather than protect it from pathogens. In Alzheimer’s Disease, the most common neurodegenerative disease, this microglia excess is even worse and is thought to contribute to cognitive decline. Since the gut bacteria are activating these potentially damaging cells, they may play a role in the progression of Alzheimer’s. Furthermore, recent research has shown that gut bacteria can produce a protein called amyloid, which is also excessively produced in Alzheimer’s. Amyloids can clump together and form large, insoluble aggregates in the brain, damaging neurons and causing the main symptoms of Alzheimer’s. Now, there are several studies looking into the benefits of probiotics, which show some potential to alter the gut microbiota in mice, on the risk and progression of Alzheimer’s in humans. To learn more, check out this blog article[3].
Why should we care? Aside from the obvious answer of expanding what we know about the body and the mind, multidisciplinary research connecting the gut and the brain could point to new treatments in a variety of areas. Many of the treatments for the most common neurological disorders, including depression, have low success rates and unpleasant side effects. New, innovative treatments that target multiple aspects of disorders (i.e., the gut and the brain) may be more successful. For example, the term psychobiotics has recently arisen to cover the clinical administration of live bacteria (probiotics) and/or molecules that promote bacterial growth (prebiotics) to improve a patient’s mental health. One company, aptly named Psychobiotics, has begun investigating the benefits of live bacteria in reducing the stress hormone cortisol in mice, which has been linked with anxiety. Check out the book by Psychobiotics CEO here[4].
Additionally, many neurological disorders have complex diagnosis processes which are largely based on behaviour – not neuroscience – which can lead to misdiagnosis. For example, the criteria for autism was proposed for the male brain, and as such many women go undiagnosed. The excess or absence of certain gut bacteria or their products could provide an earlier, more quantitative diagnostic tool to be used alongside behavioural signs, and allow people to get help sooner.
However, we’re not quite there yet with gut-brain research, and there are still many challenges to be faced. For example, many studies are done using mice, and human mental health may be too complex to be reflected in mice. Furthermore, there is an issue of the ‘chicken and the egg’ – it can be unclear whether certain bacteria cause the disorder, or if their growth is altered by having it. Likely, it is a bidirectional relationship, with both being partly true. There is also the issue of commercialisation; research into psychobiotics is often led by for-profit companies, and “promising” medications can often be released before there is solid science to explain their effects, which discredits the wider field of gut-brain research in the public’s eyes. Finally, neurodivergence is not necessarily detrimental, and there is the important question of whether we should be looking for treatments at all, or rather focusing on changing society to be more inclusive. This is a difficult question, and the answer changes from patient to patient. Regardless, studies involving the gut microbiota are providing new insights into the “why” and “how” in mental health and neurodivergence, which can only help us to better support those affected by it.
Edited by Anna Andrusaite
[1] https://www.youtube.com/watch?v=awtmTJW9ic8
[2] https://www.youtube.com/watch?v=Y4ZgAaAwPtk&t=631s
[3] https://www.brightfocus.org/alzheimers/article/gut-bacteria-and-brains-how-microbiome-affects-alzheimers-disease