Man-made brains: A tool for understanding Parkinson’s?

Around 1 in 500 people in the UK are living with Parkinson’s disease[1]. Yet, many of the exact processes involved in the progression of Parkinson’s are still unclear – with no current treatment. Man-made structures coined ‘mini-brains’ could help to change this[2]. But what is Parkinson’s? And how is this any different to research we have done in the past?
Parkinson’s disease is a progressive neurological disease characterised by low levels of dopamine, due to the loss of dopaminergic neurons[3]. The disease is highly debilitating, causing both physical and cognitive decline, which progresses until a person’s death.
Previous research has put emphasis on the use of animal brains. An animal, say a mouse, would undergo genetic modification to develop similar mutations (genetic variations) to those seen in humans with Parkinson’s. This in theory should let scientists understand how Parkinson’s progresses; but in practice, this is not the case[4]. The disease course seen in mice is different to that in humans, meaning that whilst some understanding can be gained, the usefulness of the research in terms of treating the disease is limited[5].
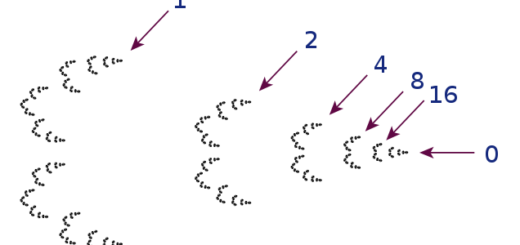
This is where ‘mini-brains’ come in. To truly mimic the progression of Parkinson’s as it is seen in the human brain, human cells are needed. These ‘mini-brains’ (known as human midbrain-like organoids[6]) are made from induced pluripotent stem cells from humans[7]. Stem cells can form several types of cells[8]. However, in this case, they are specially engineered to form the cells found in the human mid-brain (the area of the brain most involved in Parkinson’s – where the dopaminergic neurons are found). Scientists again used technology to introduce mutations associated with Parkinson’s into the mini-brains. This time, unlike with animals, the cells began to degenerate following the same patterns seen in humans with the disease[9]. This is exciting (really!). Effectively mimicking Parkinson’s in the lab gives a larger scope for further understanding the disease, and more importantly, it means that many drugs and treatments can be tested against different aspects of the disease.
A treatment for Parkinson’s is unlikely to be a one size fits all scenario. Many factors are involved in the development of Parkinson’s and its progression, and these vary between people. ‘Mini-brains’, however, provide scientists with the opportunity to isolate each of these factors over time, testing different treatments for each[10]. This may ultimately lead to treatments that can be effective in slowing or even eliminating Parkinson’s progression in humans.
Edited by Liam Butler
Copyedited by Claire Thomson
[1] https://www.nhs.uk/conditions/parkinsons-disease/
[2] https://onlinelibrary.wiley.com/doi/10.1002/ana.26166
[3] https://www.mayoclinic.org/diseases-conditions/parkinsons-disease/symptoms-causes/syc-20376055
[4] https://content.iospress.com/articles/journal-of-parkinsons-disease/jpd202200
[5] https://www.science.org/features/2018/10/replacing-replacements-animal-model-alternatives
[6] https://www.news-medical.net/life-sciences/What-are-Organoids.aspx
[7] https://www.sciencedirect.com/science/article/pii/S1934590916302004
[8] https://www.mayoclinic.org/tests-procedures/bone-marrow-transplant/in-depth/stem-cells/art-20048117
[9] https://onlinelibrary.wiley.com/doi/10.1002/ana.26166
[10] https://elifesciences.org/digests/52904/mass-producing-a-model-for-parkinson-s-disease