Our immune system & microbiome: a relationship that we should work on
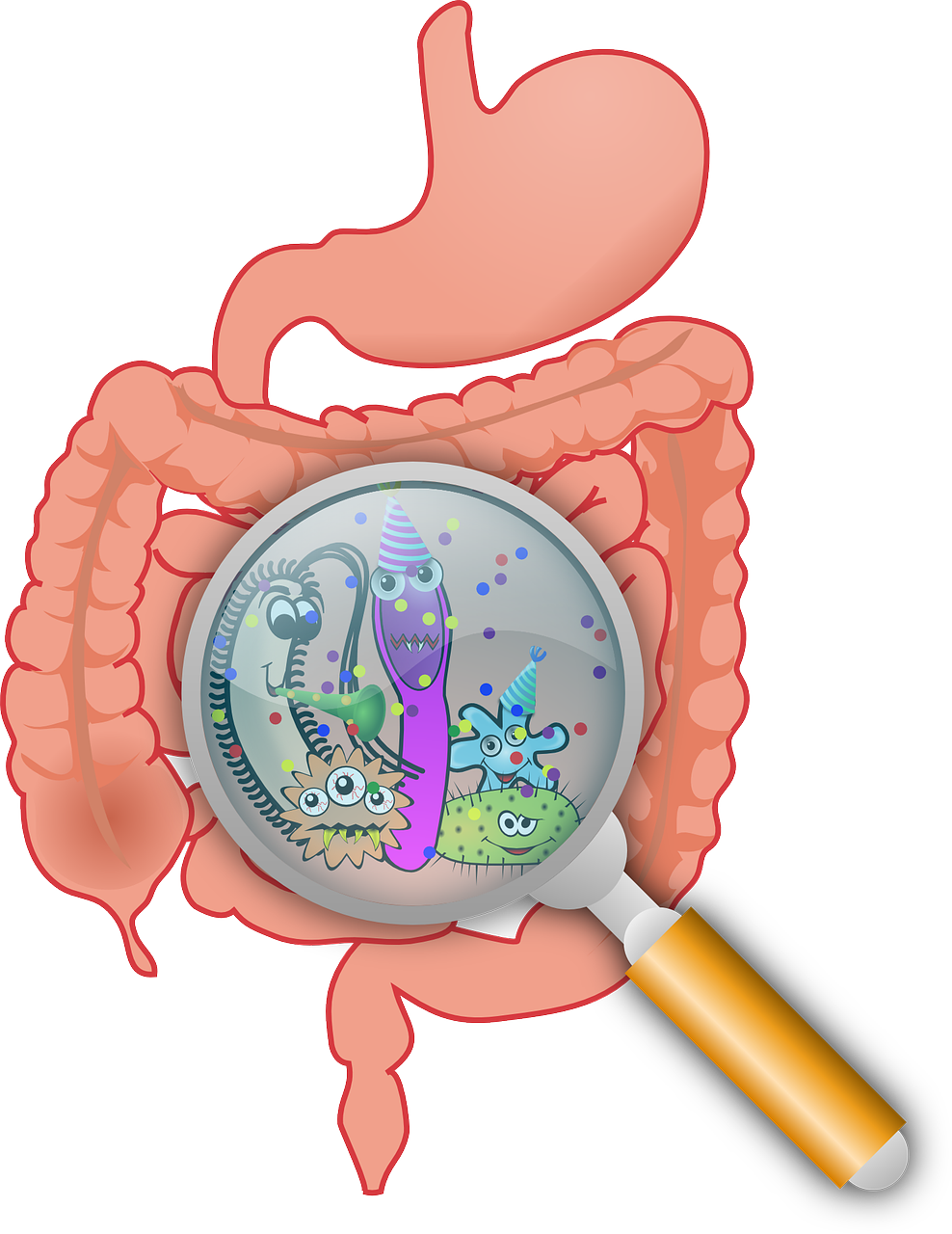
Our intestine is home to roughly 100 trillion organisms comprising of many species, including bacteria, which we refer to as the microbiome. Remarkably, these bacteria manage to live happily inside us without making us sick. Scientists have proven that the relationship between our bodies and the microbiome is not only harmonious but also vital to our health. In this article, I will explain how your microbiome plays a crucial role in your everyday life (in fact we would struggle to live without them). More importantly, I will show you what can happen if things go wrong.
The microbiome contributes to our health in a number of ways, but one of the most important interactions is between the bacteria living in our intestine and our immune system. All over our body, the immune system strives to protect us from pathogens (organisms that can cause illness). This is also true in the intestine, but due to the intestine being home to the largest number of bacteria in our body, it can be tricky. The intestinal immune system requires extra layers of regulation to allow it to differentiate between a pathogen and ‘friendly’ bacteria to keep us healthy. So what are friendly bacteria and why do we need them?
Friendly bacteria are found in many foods, including yoghurt, sauerkraut and kimchi, and include species called Lactobacillus and Bifidobacteria. The main reason that we need friendly bacteria is that they can perform jobs that our cells cannot. They are efficient at breaking down otherwise indigestible components from our diet to produce energy sources and vitamins. They produce Vitamin K which is essential for healing wounds and B vitamins that are involved in the reactions that our cells perform to produce energy from our diet.
Friendly bacteria also break down fibre. During this process, they produce molecules called short-chain fatty acids (SCFAs), which are particularly important for our intestinal immune system 1. SCFAs directly interact with immune cells, such as macrophages and T cells, via surface receptors. We directly benefit from this interaction because SCFAs dampen immune responses to intestinal bacteria to avoid harmful inflammation. When inflammation occurs, our tissue becomes swollen, red and sometimes painful due to an immune response (you’ll be familiar with intestinal inflammation if you’ve ever had food poisoning, commonly caused by a pathogen called Salmonella). This reaction is normal and actually helpful when we have an infection caused by a pathogen, but we do not want to kill and generate inflammation against friendly bacteria. The problem with inflammation is that it leads to damage of the intestine, which makes things worse as it allows bacteria to enter the tissue causing more inflammation. This type of response can lead to unpleasant symptoms such as pain and diarrhea. Basically, SCFAs mediate a signal that says “Guys, chill out and stop over-reacting. We are the healthy bacteria, and won’t cause any harm.” These are some of the reasons why we are encouraged to take antibiotics only when we need them. Antibiotics are very good at killing pathogens, but unfortunately, they also kill our friendly bacteria.
Researchers have found that the diversity of the microbiome is also crucial. A diverse community of bacteria has many species offering similar functions that we require. Taking antibiotics is harmful to the friendly bacteria in the intestine. Fortunately, a diverse microbiome can keep us healthy, because the unharmed species can take up the role of those that have been removed by antibiotics. A diverse microbiome is also good for our immune system because different bacteria promote different flavours of immune responses, which in turn maintains the balance of the immune system. Friendly bacteria also prevent infections by competing with pathogens for nutrients. Microbial diversity is highly associated with good health, so we should probably think and learn about how we can promote this diversity.
When we are healthy, we have a diverse microbiome and lots of SCFAs which helps to prevent inflammation. But you may be wondering what happens if our microbiome is unhealthy? Well, it turns out that having less SCFA-producing bacteria increases your risk of developing inflammatory bowel disease (IBD). IBD causes diarrhoea, pain and tiredness due to inflammation caused by overactive immune cells killing intestinal bacteria, including the friendly species, and causing damage to the intestine. The microbiome isn’t the only factor that influences your risk of developing IBD, your genes are important too. It’s not really clear whether people with IBD develop an unhealthy microbiome before or after they get IBD. However, giving people with IBD a healthy microbiome (via a stool transplant where you basically take a faecal sample from someone with a healthy microbiome and give it to someone with IBD) does seem to reduce inflammation for some people 2.
A lot of research surrounding the benefits of friendly bacteria focus on their importance in relation to our intestine. More recently, scientists are beginning to understand the importance of the microbiome in relation to other organs, such as the brain. An unhealthy microbiome has been linked to Alzheimer’s disease 3 and depression 4. This finding is fascinating as scientists are predicting that understanding how the microbiome interacts with the brain could help us develop new treatments for many illnesses. The intestine and the brain have many ways in which they communicate, such as through the vagus nerve (a large nerve composed of fibres connecting the brain to the intestine) and indirectly via substances from the intestine that reach the brain via the blood. This area of science, referred to as the gut-brain axis, is rapidly developing but is challenging because it is difficult to prove that what goes on in the intestine can directly influence the brain. In the coming years, it is predicted that we might be able to target some mental health illnesses, such as depression, by changing our microbiome.
At present, it’s clear that the best way to change your microbiome is through diet. So how can you adapt your diet to promote a healthy microbiome? A typical western diet consisting of high fat, processed meat and low vegetable intake reduces microbiome diversity and SCFA production. If you have this diet you are more likely to develop IBD. For now, the best advice for promoting a healthy microbiome and thus a healthy immune system is to have a colourful diet full of vegetables, fruit, fish, grains, and nuts 5.
There is so much compelling evidence to convince us why we need to keep our microbiome healthy. The saying “you are what you eat” has never been truer, or maybe “you are what your microbiome eats” would be more accurate. As technology and our understanding of the health benefits of our microbiome develop, it’ll become clearer how we can modulate our bacterial species to prevent disease and promote health. Like any collaboration, it can be complicated and issues can arise, but when it works it can promote beautiful results.
This article was specialist edited by Ricardo Sanchez and copy-edited by Dzachary Zainudden.