Transpoosions: The World Of Poo Transplants

Doctors, researchers and hospital bureaucrats have long sought a wonder drug; a cheap, readily available treatment for a multitude of conditions. It turns out that such a thing might just exist, and that it might well be poo. It sounds counter-intuitive, perhaps, given the fact that, well, it’s poo, but faecal microbiota transplants (FMT) are looking to be a fantastic treatment of the future. So what are they?
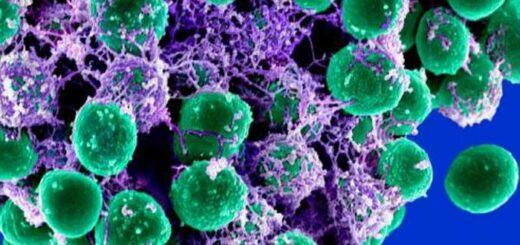
Microbiota refers to the collection of bacteria and other microorganisms living in our gut. FMT, or transpoosions, as it is sometimes jokingly called, involves taking a sample of stool from a healthy donor and inserting it into the intestine of the receiver, in the hope of restoring the microbiota by encouraging ‘good’ bacteria to grow. Inserting how? I’m glad you asked. Originally FMT was carried out by faecal enemas, but now can be administered by colonoscopy or as the world’s worst milkshake. The donor stool is liquefied with saline solution and delivered either rectally via endoscope, or by nasointestinal tube (a tube going into the nose and down to the small intestine), fortunately requiring no tasting.
We’ve all seen the adverts for yogurts containing ‘friendly bacteria’, which will happily colonise our intestines and free us from bloating. In our guts, our new chums would be joining the ranks of approximately 1014 (that’s 100,000,000,000,000) microbiota that call our digestive tracts home. It is worth noting that that’s ten times higher than the number of human cells in our bodies. The role of intestinal microbes has not yet been fully explored, but they have been shown to play a significant part in digestion and energy metabolism, such as helping digest plant fibre and producing vitamin K and some B vitamins. Additionally, they have been shown to influence the development and progression of diseases such as Crohn’s disease and irritable bowel syndrome, and are potentially implicated in the development of some autoimmune and metabolic disorders 1. The overall function of gut bacteria is determined largely by the proportion of different species present, and for our health we rely on the helpful and neutral species out-competing the less helpful and detrimental ones. When imbalances occur it can have dire consequences. An example of this is Clostridium difficile infection, which has a garnered a significant amount of attention, due to the extremely unpleasant nature of the symptoms and the fact it occurs largely in people receiving hospital treatment, though the number of cases outside of healthcare settings is growing.
C. difficile can be present as part of a normal gut bacteria colony, but if a large proportion of other species are destroyed (as occurs through broad-spectrum antibiotic treatment) it will multiply quickly and take over. The bacteria release toxins causing diarrhoea, abdominal cramps and fever, and can cause a build up of gas resulting in the potentially life-threatening and painful swelling of the bowel, called toxic megacolon 2. Although many cases can be treated by withdrawing antibiotic treatment (allowing destroyed species to repopulate) or through strong antibiotic treatment in more severe cases, some patients suffer from recurring infections, with the chance of recurrence increasing with each subsequent infection. FMT has been used successfully to treat recurrent and moderate treatment-resistant C. difficile infections, with donor bacteria persisting in the recipients’ gut for up to twenty four weeks, as shown by Dr Martin Grehan of Nepean Hospital, New South Wales 3.
Another significant and promising application of FMT is in the treatment of obesity and related diseases. While many people disregard obesity as simply a matter of too much food and too little exercise, the disease can actually be far more complicated, involving various hormonal and genetic factors, and, as is becoming apparent, the gut microbiota. One study, by Dr Lee Kaplan of Massachusetts General Hospital, Boston, involved transplanting microbes from obese mice who had been given gastric bypass surgery into mice who lacked their own gut microbes. The recipient mice subsequently experienced a 5% drop in weight, which might be explained by changes in the microbiota of the donor mice following their gastric bypass surgery. 4. The complex interplay of factors is further demonstrated by another study by Dr Jeffrey Gordon of Washington University, St. Louis, which gave different groups of mice human faecal samples from sets of twins, in which one was lean and the other obese. Mice given the obese twins’ samples went on to gain weight, despite eating similar amounts of food as the lean mice. Dr Gordon’s group also investigated the effect of diet on gut microbiota, and demonstrated that a diet high in fruit and vegetables and low in saturated fat was more conducive to maintaining beneficial bacterial species than a diet low in fruit and vegetables and high in saturated fat 5.
Obesity is one of the component diseases of metabolic syndrome, an energy utilisation and storage disorder which greatly increases the risk of death from cardiovascular causes. Dyslipidaemia (abnormal levels of fats in the blood), and diabetes, or the precursor, reduced insulin sensitivity (a reduction in the body’s response to insulin, resulting in higher blood sugar levels) are other major components of the syndrome. A study by Anne Vrieze, a medical doctor and PhD student at Wageningen University, Netherlands, demonstrated that men with metabolic syndrome exhibited decreased fat levels in the blood and improved insulin sensitivity when treated with faecal transplants from lean donors 6.
These studies are extremely strong indicators of the potential of FMT and that the role of the gut microbiota may be far more extensive than previously thought. Though they are far from solid evidence that we should be asking for FMT to cure all our ills, that hasn’t stopped a number of long-suffering patients with chronic illnesses from seeking out the treatment, which is available at a relatively small number of clinics and hospitals across the globe. Access is limited somewhat by regulatory issues. In the USA in particular, the Food and Drug Administration has been slow to embrace the transpoosion, with cumbersome regulation reducing the availability of the procedure. Similarly in the UK, very little seems to be said about the procedure and few doctors have stated that they carry out the procedure. This reluctance on the part of national bodies is resulting in people seemingly turning to the proverbial back-alley, or even the DIY option, and of course, instructions are available online. While it is possible for an unregulated procedure to be safe, there are no guarantees, and little option for recourse should things go badly. Perhaps the population as a whole has not got over the ‘ickiness’ of FMT, but, as Professor Thomas Borody of the Centre for Digestive Disease, Sydney, reports, people who have suffered for years with C. difficile, ulcerative colitis and other such conditions, do not seem to have any qualms with trying it out.
Overall, it would seem that there is great potential for FMT to help a large number of people and to ease a great deal of suffering. Hopefully as the practice is refined and further research is done into the role of gut microbes and their interactions with the body, we will be able to overcome the ‘yuck’ factor and solve more medical problems with transpoosions.
References
- Borody TJ and Khoruts A. Fecal microbiota transplantation and emerging applications. Nature Review Gastroenterology and Hepatology. [Online]. 2011; 9(2012): 88-96.
- NHS Choices. Clostridium difficle.
- Grehan MJ, Borody TJ, Leis SM, Campbell J, Mitchell H and Wettstein a. Durable alteration of the colonic microbiota by the administration of donor fecal flora. Journal of Clinical Gastroenterology.
- Liou AP, Paziuk M, Luevano Jr J-M, Machineni S, Turnbaugh PJ and Kaplan LM. Conserved shifts in the gut microbiota due to gastric bypass reduce host weight and adiposity. Science Translational Medicine. [Online]. 2013; 5(178): 178ra41.
- Riduara VK, et al. Gut microbiota from twins disconcordant for obesity modulate metabolism in mice. Science. 2013; 341(6150).
- Vrieze A, et al. Transfer of Intestinal Microbes From Lean Donors Increases Insulin Sensitivity in Individuals With Metabolic Syndrome. Gastroenterology. 2012; 143(4): 913-916.e7.