Catching Cancer: The Viruses that Transform Cells into Tumours
Viruses are invaders of our cells, hijacking the machinery contained within for their own means, and then bursting out once they’re done, leaving a slew of damage and disease in their wake. This relationship is not a new one: they have evolved alongside us, and in fact, they don’t only infect humans. There are viruses that prey on every living being on earth, right down to the smallest bacteria. There is no shortage of them either; the 1 x 1031 viruses present on our planet would cover the distance from Earth to the Sun 1,500 times if they were arranged next to one another1. But you don’t have to be a virologist to have an awareness of them as they have a huge impact on our lives; from the rhinovirus that causes the common cold, to the H1N1 influenza virus that was at the heart of both the devastating Spanish flu pandemic in 1918 (responsible for more deaths than both the world wars combined)2 and the global swine flu scare of 2009. However, there remains a subset of viral pathogens that remain relatively unknown to the general public, which is surprising considering the role they play in one of the most devastating diseases that afflicts our species. These are the oncoviruses and they have the potential to cause cancer — the ‘C’ word that strikes fear into many. In fact, they are the cause of between 10-12% of cancers worldwide, with that figure heightened to 45% in Sub-Saharan Africa, the most affected region. However, the viral root of these cancers means that they have the potential to be prevented if a vaccine against the causative agent can be produced, making this a vital line of research. We have now known about oncoviruses for over 50 years; however, the field is continually expanding, with the most recent member, Merkel cell polyomavirus, being added to the group within the last few years.
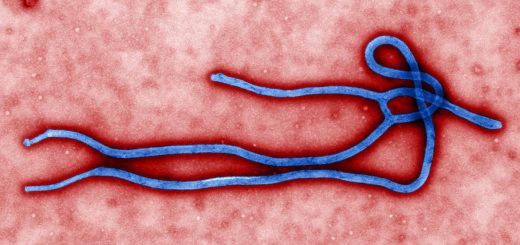
Scientists have pondered the idea of infectious agents being at the heart of the development of certain cancers since the role of infectious bacteria in chronic conditions, such as tuberculosis, came to light in the late 1800s. By 1911, Peyton Rous had made the discovery that a tumour present in chickens could be transmitted from a diseased individual to a healthy one through the transfer of tumour extracts, suggesting that some kind of transmissible agent was causing the disease3. Years later, in 1933, the structure of this agent could finally be visualised, using the newly invented electron microscope. It was identified as a virus and named the Rous sarcoma virus (RSV) in honour of its discoverer.
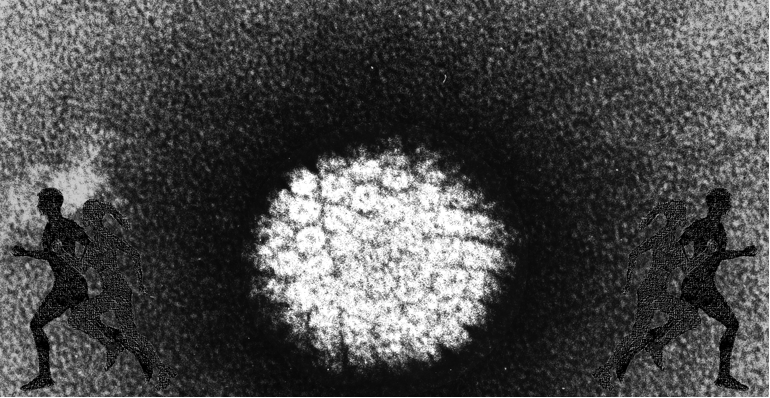
Even though additional tumour-inducing viruses were found in animals after Rous’ discovery, the scientific community widely shunned the concept of viral pathogens causing cancer in humans due to our heightened molecular complexity. This did not deter a young researcher, Anthony Epstein, who was committed to finding a human cancer caused by a virus4. Inspiration arrived in 1961 when he attended a lecture by a surgeon, Denis Burkitt, who had identified a unique tumour of the jaw, later coined Burkitt’s Lymphoma, which was common in children in Uganda. What evoked Epstein’s curiosity was that Burkitt’s Lymphoma seemed to be confined by geographical boundaries and temperature, in that it was specifically found in African regions located at the equator, where temperatures were maintained above 15°C throughout the entire year. These limitations suggested an infectious origin, and immediately he knew that this was the tumour he had been looking for. Sure enough, Epstein and his team found a never-before-seen virus, now known as the Epstein-Barr virus (EBV), in the Burkitt’s Lymphoma tumour cells. EBV is so-called for Epstein himself and for Yvonne Barr, who was a PhD student under Anthony at the time. They identified it as belonging to the herpesvirus family, which counts the viruses responsible for cold sores and chicken pox as being amongst its members. Subsequently, a link between EBV and several other cancers, including Hodgkin’s Lymphoma, was also found.
It is now known that EBV is a ubiquitous infection, with over 90% of people infected with the virus by the time they reach their twenties5. Most individuals contract EBV during their early childhood years and don’t display any symptoms. However, the virus is not cleared by our immune system. It persists in a type of white blood cell, called B cells, that are a key component of our memory immune response, which tackle infections that our bodies have previously been exposed to6. Whilst the virus lies latent inside these cells, it displays certain proteins on the cell surface. When these proteins are present at an unusually high level they are recognised by another group of cells from the immune system, cytotoxic T cells, as a sign that something is wrong and the infected cell is killed. This management of infected cells is usually sufficient and explains why most of our population carries EBV but does not develop associated cancers. It is when our immune system loses control that problems arise. In the case of Burkitt’s Lymphoma, the increased viral protein levels promote the cell to make copies of itself at an unregulated rate. During this proliferation, new copies are made of the cells’ DNA — the genetic material that contains all the instructions the cell needs to survive. Critical to the development of cancerous cells are the changes that are made to the DNA whilst these copies are being created. A specific sequence of DNA, or gene, called Myc, is removed from its position and relocated elsewhere in the genome. This tampering frees the cells from regulation and allows them to dramatically increase their copy numbers and avoid destruction by the repair mechanisms usually employed. These changes result in the formation of tumours made up of the transformed cells.
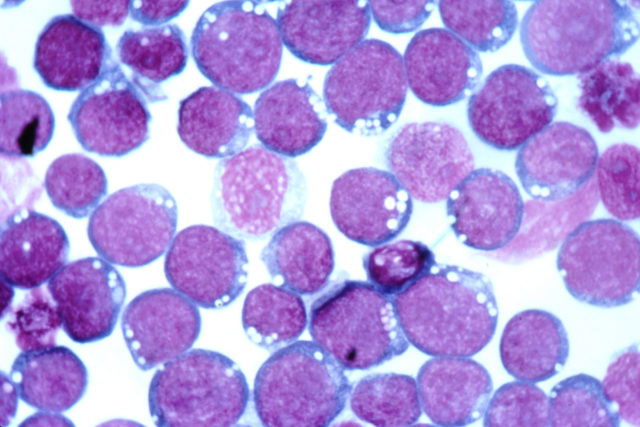
Since the discovery of EBV, six other viruses that induce tumours in humans have been discovered, including human papillomavirus (HPV), each with its own way of disrupting the usual cellular processes to transform it into a cancerous cell7. The HPV group is made up of numerous variants, with at least 13 of them being classified as ‘high-risk’ due to their carcinogenic capabilities. Two HPV types, HPV16 and HPV18, cause 70% of cervical cancers and because of this, HPV infections are a particular worry for females8. However, due to their ability to also cause cancers affecting other areas of the body, the threat they present transcends gender. Similarly to EBV tumorigenesis, an inability to effectively clear the HPV infection can lead to cancer. At this point, the virus changes the morphology of the cells it has infected, forming what are called ‘precancerous lesions’ and these are what doctors look for in females during regular cervical screenings or ‘smear tests’. These irregularities can be removed early on before they develop into cancer. If they are left to progress, HPV will actively disrupt usual tumour suppression mechanisms in the host cells, allowing them to continue uninterrupted on their path to becoming cancerous9.
In women under 35 in the UK, cervical cancer is the most common form of cancer. As is often the case, the plight is even worse in developing countries; 84% of new cases of cervical cancer worldwide affect women in these nations. The story of HPV and cervical cancer is not all doom and gloom however, as the situation is turning around. A vaccine against four types of HPV, including HPV16 and HPV18, was developed and implemented in the UK immunisation schedule as of 200810. It is administered to all girls between the ages of 12 and 18 and has been very effective in reducing rates of precancerous lesions, caused by the two high risk types it covers, by 99%. There is also a new form of the vaccine expanded to protect against an extra five types of HPV; however, it is currently only available privately. Unfortunately, huge obstacles still exist regarding the rollout of the vaccine in developing countries, where it is needed the most. A full course of the vaccine costs $300, making it hugely expensive. However, in 2011, Rwanda successfully introduced a vaccination programme, the first developing country to do so, which was made possible by a donation of the vaccine given by the production company11. It is hoped that more African countries will follow suit, especially with the renewed support from the Global Alliance for Vaccines and Immunisation, an organisation set up by the Bill & Melinda Gates Foundation in partnership with the World Health Organisation to promote “access to immunisation in poor countries”.
Cancer is arguably the most complex disease that plagues humanity and thus it is uncertain whether an all-encompassing cure for its many branches will ever be found. Attempting to tackle the cancers caused by these oncoviruses presents a much more achievable goal. It is known that viral infections can be prevented with the development of effective vaccines and with the production of more vaccines against oncoviruses, like the successful HPV immunisation, and the integration of them into vaccine schedules worldwide, the elimination of the threat posed by oncoviruses is within reach.
This article was specialist edited by Ricardo Sanchez Velazquez and copy-edited by Lucy Silcock.
References
- https://www.nature.com/articles/nrmicro2644
- https://www.theguardian.com/world/2018/sep/09/spanish-flu-pandemic-centenary-first-world-war
- https://www.nobelprize.org/prizes/medicine/1966/rous/biographical/
- Cancer Virus: The Story of Epstein-Barr Virus by Dorothy H. Crawford, Alan Rickson & Ingólfur Johannessen
- https://www.sciencedaily.com/releases/2017/02/170213131346.htm
- https://www.sciencedaily.com/releases/2003/11/031119081205.htm
- https://www.cancer.org/cancer/cancer-causes/infectious-agents/infections-that-can-lead-to-cancer/viruses.html
- https://www.cancer.org/cancer/cancer-causes/infectious-agents/hpv/hpv-and-cancer-info.html
- https://www.sciencedaily.com/releases/2018/03/180302091014.htm
- https://www.nhs.uk/conditions/vaccinations/hpv-human-papillomavirus-vaccine/
- https://www.who.int/bulletin/volumes/90/8/11-097253/en/