The threat posed by infectious diseases caused by viruses, bacteria and parasites in less economically developed countries is astronomical, leading to an estimated 15 million people dying every year1. Although the best healthcare intervention has always been vaccination (the eradication of smallpox is still remembered as one of the best healthcare achievements today), the traditional methods of vaccination can be problematic in some areas of the world.
The only available vaccines that protect against infectious diseases are either infectious agents that have been killed or pathogens that have been changed in some way to remove their ability to cause disease. These vaccines include an antigen, which is a protein or a molecule from the pathogen that induces an immune response but does not lead to an actual infection. This creates a memory of the specific infection. When the same pathogen infects the body at a later time, the immune system therefore remembers and generates a more robust and faster response.
These vaccines are often expensive to produce, and they are difficult to both administer and store in rural communities. They can also be dangerous, as seen in mass polio vaccination schemes in Nigeria which led to a large-scale outbreak of polio that still exists today. The outbreak was caused by the altered virus within the vaccine reverting to the pathogenic and disease-causing state when injected into the human body, thus causing infection and disease2. These risks and difficulties surrounding traditional injected vaccinations have driven the development of an edible vaccine for over thirty years.
While the theoretical concept of an edible vaccine is an economic and social success, can we express an antigen in a plant cell? And how does it induce the protective immune response needed for vaccination?
Edible vaccines can be engineered in different ways. We could integrate the genetic information of the antigen into the plant’s own genome, leading to the production of “transgenic” plants which express antigen in their leaves. This process has been successfully demonstrated within labs all over the world with different antigens of different infectious diseases. Problems arose, however, with the amount of antigen produced being too low to generate an effective immune response. Also, the generation of the transgenic plants consumed a great deal of expense and time3. These two technical issues have also added to a wider fear that these plants are “genetically modified foods” and has slowed funding to a trickle so that no edible vaccine has been licenced thus far.
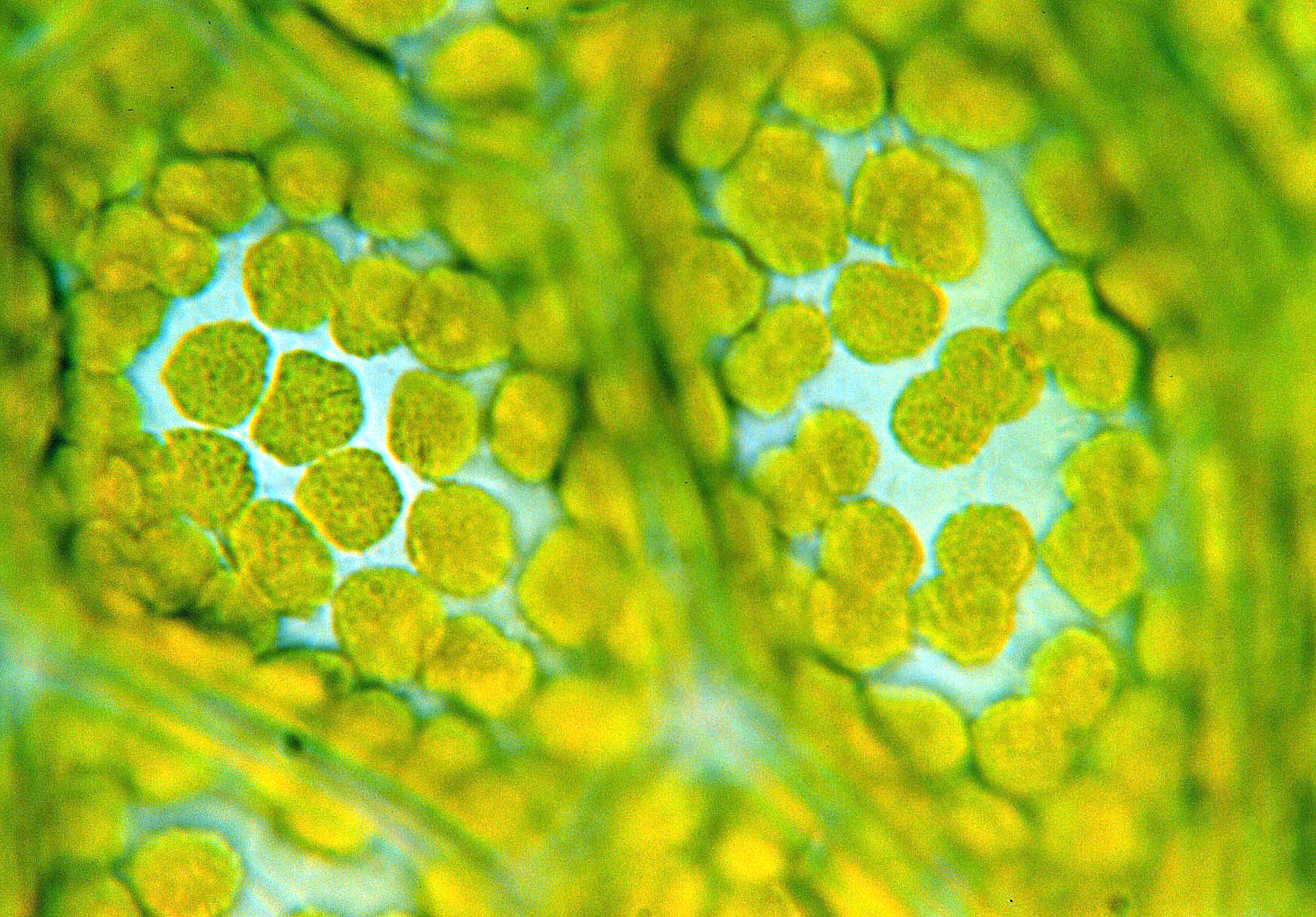
In the absence of the technical difficulties faced in development, edible vaccines have theoretical brilliance. Vaccinating through ingestion generates a far more robust immune response than a vaccine injected directly into the bloodstream since most pathogens target our mucosal surfaces such as our guts and airways4. An antigen within an eaten transgenic plant is shielded from destruction by the harsh acidic environment of the stomach by being “bioencapsulated” by plant cells that are digested later in our gastrointestinal (GI) tracts.
In humans, plant cells are broken down in our intestines by our healthy gut bacteria. The digestion of the plant cells releases the antigen which is noticed by the cells lining the mucosa of our guts5. The gut cells recognise the antigen as foreign and present it to the white blood cells of the immune system, mounting the initial immune response and releasing antibodies that quickly target and destroy any antigen they find6. This immediate immune response generates memory cells that survive within us for either entire lifetimes or until a vaccination boost is needed to ensure that a quick and strong response is stimulated when a true infection occurs.
What edible vaccines lack, however, is assistance to ensure the antigen is recognised by gut cells and that an immune response is stimulated. This assistance is often called an adjuvant. Without this assistance, there is a risk that the antigen would establish no immune response7. In current edible vaccine research, a subunit of the bacterial cholera toxin is often used as an assisting adjuvant8. Fusing the antigen and the cholera toxin subunit together makes sure that the antigen is presented to the white blood cells of the immune system.
What plants can be used for vaccination?
Plants and crops such as rice, potatoes, lettuce, and tomatoes are cheap and easy to grow. The production of an antigen within their cells does not require expensive and labour-intensive production. They also do not require cold storage or sterile injection that typical vaccines do. Without the need for injection, there is no associated pain or risk of contamination from blood borne diseases such as HIV and Hepatitis B. Since these plants are locally grown in hot countries or can be freeze-dried, cold storage is no longer a problem. Actually, it has been shown that freeze-drying the leaves of these transgenic plants increases the amount of the antigen per gram of leaf.
In hot countries there are so many plants grown as crops that can easily be genetically manipulated to become edible vaccines and survive storage. Several stand out; bananas are eaten raw and often liked by children, but trees take time to grow and the fruit spoils rapidly. Potatoes are another crop that have historically been easy to use in the lab and survive long periods of time without rotting. The downside of using potatoes as a vaccine, however, is the cooking required prior to eating which has the potential to destroy any antigen expressed within the potato. Leafy greens such as lettuce are filled with water and can easily undergo the freeze-drying process that makes them one of the best plants to use. Therefore, salad leaves appear to be the best option at this time.
Success and the future
Currently there have been no successful edible vaccines in clinical trials, but scientists have developed several candidates for edible bacterial, viral and parasitic vaccines. An interesting example is the development of the plant-derived vaccine against Bacillus anthracis, the bacteria that causes anthrax. An antigen was produced in tobacco plant leaves and injected into mice9. With the vaccine, the mice survived a lethal infection of anthrax. This vaccine, however successful, had to be injected to induce a strong enough immune response to fight against future anthrax infection. With the real goal of plant-derived vaccine research being that the vaccines are ingested rather than injected, this example illustrates that much more research is needed before any success occurs.
If science can overcome the barriers surrounding the generation of an edible vaccine, that elicits a strong enough immune response, and the fears related to genetically modified foods, edible vaccines could be the best solution for so many people facing the risk of death from infectious disease. With no edible vaccine against infectious disease currently progressing through clinical trials, however, it will take more than a few years until we are having our vaccines with our dinner.
This article was specialist edited by Bhoomi Gor and copy edited by Jessica Bownes.
References
- Daniell, H., Singh, N.D., Mason, H., Streatfield, S.J., 2009. Plant-made vaccine antigens and biopharmaceuticals. Trends in Plant Science, [online]. 14 (12), p. 669-679. Available at: DOI: 10.1016/j.tplants.2009.09.009
- Chan, H.T., Daniell, H., 2015. Plant-made oral vaccines against human infectious diseases – Are we there yet? Plant Biotechnology, [online]. 13 (8), p. 1056-1070. Available at: DOI: 10.1111/pbi.12471
- Lakshmi, P.S., Verma, D., Yang, X., Lloyd, B., Daniell, H., 2013. Low Cost Tuberculosis Vaccine Antigens in Capsules: Expression in Chloroplasts, Bio-Encapsulation, Stability and Functional Evaluation In Vitro. PLOS, [online]. 8 (1), p. 5470. Available at: DOI: 10.1371/journal.pone.0054708
- Tacket, C.O., 2007. Plant-Based Vaccines Against Diarrheal Diseases. Transactions of the American Clinical and Climatological Association, [online]. 118, p. 79-87
- Martens, E.C., Lowe, E.C., Chiang, H., Pudlo, N.A., Wu, M., McNutty, N.P., Abbot, D.W., Henrissat, B., Gilbert, H.J., Bolam, D.N., Gordon, J.I., 2011. Recognition and Degradation of Plant Cell Wall Polysaccharides by Two Human Gut Symbionts. PLOS Biology, [online]. 9 (12), p. 1001221. Available at: DOI: 10.1371/journal.pbio.1001221
- Azizi, A., Kumar, A., Diaz-Mitoma, F., Mestecky, J., 2010. Enhancing Oral Vaccine Potency by Targeting Intestinal M Cells. PLOS Pathogens, [online]. 6 (11), p. 1001147. Available at: DOI: 10.1371/journal.ppat.1001147
- Pascual, D.W., 2007. Vaccines are for dinner. PNAS, [online]. 104(26), p.10757-10758. Available at: DOI: 10.1073/pnas.0704516104
- Limaye, A., Koya, V., Samsam, M., Daniell, H., 2006. Receptor-mediated oral delivery of a bioencapsulated green fluorescent protein expressed in transgenic chloroplasts into the mouse circulatory system. FASEB, [online]. 20 (7), p. 959-961. Available at: DOI: 10.1096/fj.05-5134fje
- Koya, V., Moayeri, M., Leppla, S.H., Daniell, H., 2005. Plant-Based Vaccine: Mice Immunized with Chloroplast-Derived Anthrax Protective Antigen Survive Anthrax Lethal Toxin Challenge. Infection and Immunity, [online]. 73(12), p. 8266-8274. Available at: DOI: 10.1128/IAI.00050-08